4 Hidden Warning Signs Of Chronic Inflammation (And The 30 Day Fix)
Feb 17, 2026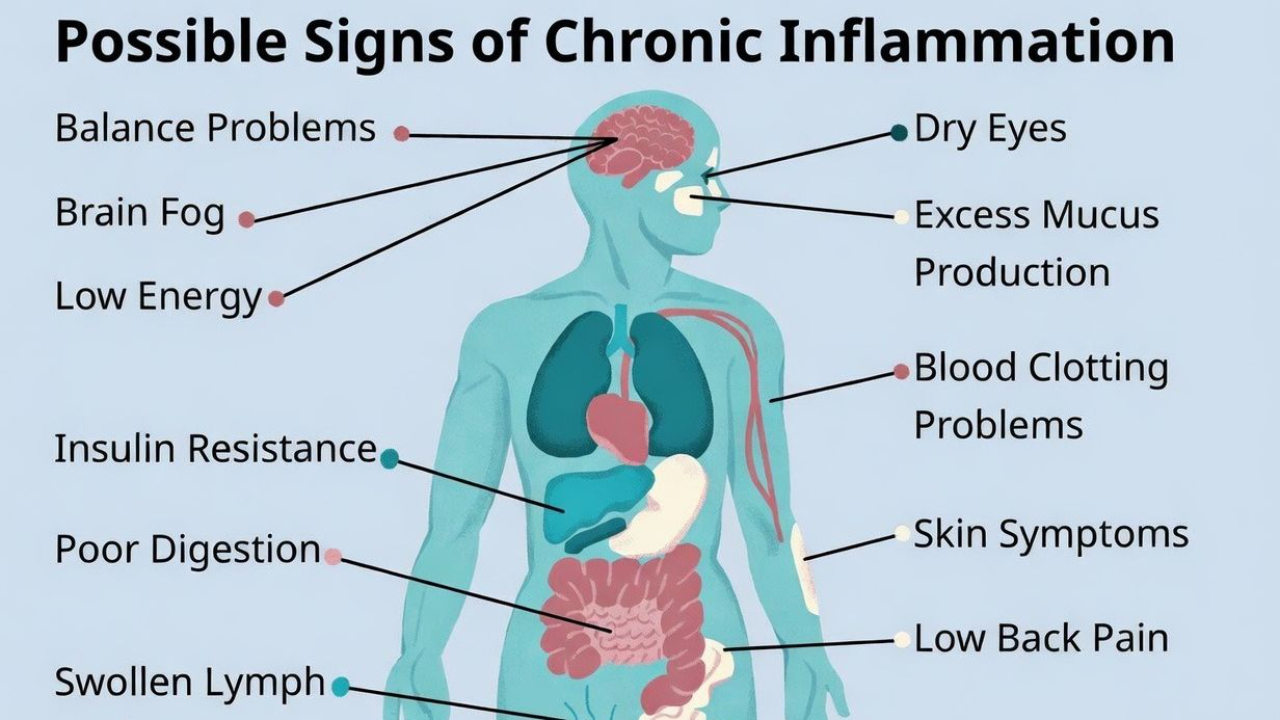
The High Performance Journal Written By Dan Go - February 17th, 2026
Past week, I've been on vacation, living in an Airbnb. In this condo, there are a lot of 60 and 70-year-olds. Retired execs and a couple of entrepreneurs who have built and sold companies.
Great people and lots of interesting conversations at the pool.
But there's one thing I can't unsee: Highly inflamed aging bodies.
Belly fat that won't budge, skin issues, and people having difficulty walking due to chronic pains that will only get worse as they get older.
Last week, I was chatting with one of my neighbours who's semi-retired, and I asked him about a patch he was wearing on his shoulder. He mentioned that his arthritis was flaring up again, and it was helping him relieve it.
The conversation got to what I did for work, and I told them, "I help entrepreneurs get lean and healthy with ease and minimal stress."
He laughed. "So you probably know all about this stuff."
"I deal with it all the time, but I work on preventing these things from ever happening", I replied.
As we got into it, I opened his mind to the fact that arthritis isn't just a joint problem; it's a sign of high inflammation.
His expression changed. "That's what my GP said to me when he saw my blood work, but no one ever told me what to do about it."
And unfortunately, most people don't realize they're inflamed until something breaks.
The body sends warning signs for years; we just don't know what to look for.
What Is Inflammation (And Why Should You Care)?
Before getting into it, I have to mention that inflammation isn't always a bad thing. It's your body's natural defence system.
It's an oversimplification, but when you work out, your muscles get inflamed; your body goes to help them recover, and you gain muscle.
Just the other day, I was surfing, and I jumped off a wave and accidentally hit my chin on my board, and it started swelling. That's acute inflammation doing its job.
The problem is chronic inflammation. It's low-grade, constant, and invisible. For many people, it simmers in the background for years, quietly damaging their arteries, joints, brains, and organs.
Research links chronic inflammation to heart disease, diabetes, cancer, Alzheimer's, and accelerated aging.
It's the common thread behind almost every disease that takes people down after 40. The scary part is you can have it for years and still feel "fine."
4 Hidden Warning Signs You're Chronically Inflamed
1. Bleeding Gums
I dealt with this one when I was younger. You brush your teeth, and when you spit, you see pink in the sink. Now, most people ignore this, but bleeding gums are a sign of periodontal inflammation, and this correlates with systemic inflammation throughout your body
2. Skin Issues (Dermatitis, Eczema, Psoriasis)
Your skin is a mirror of what's happening inside. Chronic skin flare-ups aren't just a surface problem. They're your body raising an alarm that something deeper is off.
3. Stubborn Belly Fat
Visceral fat, the fat around your organs, doesn't just make your belly stick out. It's metabolically active and pumps out inflammatory chemicals 24/7. If your midsection won't budge no matter what you do, inflammation might be the culprit.
4. Any "itis"
Arthritis. Tendinitis. Bursitis. Colitis. If it ends in "itis," it means inflammation. These aren't random. They're symptoms of a body on fire.
How To Check Your Inflammation Levels
Before you fix it, measure it. Ask your doctor or do a functional blood test looking for these markers:
- hs-CRP (high-sensitivity C-reactive protein): The gold standard for systemic inflammation. Under 1.0 mg/L is ideal. Over 3.0 is high risk.
- Fasting insulin: High insulin often travels with high inflammation.
- Homocysteine: Elevated levels indicate inflammation and cardiovascular risk.
Get your baseline. If it's in the danger zone, do the protocol below, then retest.
The 30-Day Inflammation Fix Protocol
Pillar 1: Anti-Inflammatory Nutrition
What you eat is a major lever in your fight against inflammation. Every meal is an asset or liability. Every piece of food you put in your mouth is either feeding or fighting it.
- Cut ultra-processed foods and added sugars. They're gasoline on the fire.
- Avoid processed meats (bacon, sausage, deli meat).
- Cook with extra virgin olive oil. It's loaded with anti-inflammatory polyphenols.
- Eat fatty fish 2-3x per week (salmon, sardines, mackerel). The omega-3s (EPA/DHA) directly lower inflammatory markers.
- Add polyphenol-rich foods: berries, leafy greens, green tea, dark chocolate.
- Use spices liberally: turmeric, ginger, garlic, and rosemary.
- Hit 25-35 grams of fiber daily. Your gut microbiome controls more inflammation than you think.
- Maintain a mild calorie deficit (10-20%) if you have fat to lose. Less visceral fat = less inflammation.
Pillar 2: Low-Intensity Movement
Inflammation is a sign of chronic stress, and one of the best ways to fight chronic stress is to walk a lot, aiming for 8,000 to 10,000 steps daily.
You want to do this especially after meals, because this is a powerful way to regulate your blood sugar and inflammation.
Also, skip the chronic cardio. You can actually increase inflammation if you're already stressed. Walking is anti-inflammatory. Running yourself into the ground is not.
Pillar 3: Circadian Alignment
Your body runs on a 24-hour clock. When your sleep, light exposure, and meal timing are misaligned, you create circadian dysfunction, and inflammation rises.
- Get morning sunlight within 30-60 minutes of waking. This sets your circadian rhythm and improves sleep quality later.
- Dim lights and reduce screens 1-2 hours before bed.
- 7-9 hours of quality sleep. Consistent sleep and wake times. Your body loves rhythm.
- Front-load your calories earlier in the day when possible and set a hard stop for your final meal 3-5 hours before bed.
- Cool, dark bedroom. No large meals or caffeine 10 hours pre-sleep.
Pillar 4: Stress Management
Chronic stress is one of the biggest drivers of low-grade inflammation. You can't out-supplement or out-exercise a fried nervous system.
- Daily stress-down practice: 10-15 minutes of breathing, meditation, or a walk outside.
- Build a recovery routine into your schedule, especially after work.
- Identify your top 2-3 stress triggers and create boundaries around them.
- Get outside daily. Nature exposure lowers cortisol and inflammatory markers.
- If you're always "on," your inflammation will be too.
Supplements And Non-Obvious Ways to Reduce Inflammation
Once your foundations are solid, these additions can accelerate results. Some are supplements. Some are habits most people overlook.
- Omega-3 (EPA/DHA): 2-3 grams daily. Proven to reduce systemic inflammation.
- Probiotics: Certain strains (like L. reuteri) have shown reductions in hs-CRP.
- Vitamin D3: If you're not getting enough sun, supplement. Low Vit D correlates with higher inflammation.
- Magnesium: Most people are deficient. It plays a role in over 300 enzymatic reactions, including inflammation regulation.
- Oral hygiene: Your mouth is the gateway to systemic inflammation. Periodontal disease is one of the most underappreciated sources of chronic inflammation.
- Sauna or heat exposure: Heat stress triggers heat shock proteins that help reduce inflammation.
- Cold exposure: Cold showers or ice baths lower inflammatory markers and improve circulation.
- Nasal breathing: Mouth breathing increases inflammation and disrupts sleep. Tape your mouth at night if needed.
- Limit alcohol: Even moderate drinking increases gut permeability and inflammatory markers. Less is better.
Your 30-Day Action Plan
Here's how to put this together:
Week 1: Assess and Eliminate
Get your blood work done (hs-CRP, fasting insulin, homocysteine). Remove ultra-processed foods, added sugars, and processed meats. Start walking 8,000 steps daily. Upgrade your oral hygiene.
Week 2: Add and Build
Fatty fish 2-3x per week. Polyphenol-rich foods and anti-inflammatory spices daily. Lock in your sleep schedule. Morning sunlight within an hour of waking. Start omega-3 and vitamin D.
Week 3: Optimize
Hit 25-35g fiber daily. Add a 10-15 minute daily stress-down practice. Introduce sauna or cold exposure. Cut back on alcohol. Practice nasal breathing.
Week 4: Sustain and Measure
Keep the habits running. Notice how you feel. Schedule your 90-day retest to see your markers move.
Get More "Good" Inflammation And Banish The "Bad".
Again, I want to point out that inflammation isn't bad. In acute situations, it can actually help.
But chronic inflammation doesn't announce itself. It accumulates silently for years. Inflammation doesn't announce itself. It accumulates. Silently. For years.
Then one day you get a diagnosis, and everyone acts surprised.
Don't wait for the wake-up call. Get your blood work. Follow the protocol. Give it 30 days.
Your future self will thank you.
Onward and upward. 🚀
- Dan
When you're ready, here are 2 ways I can help:
1. The Lean Body 90 System: When you’re ready to get in great shape, Lean Body 90 is the obvious choice. You can get in great shape and reach your fitness goals in just 90 minutes a week. Lose weight and build muscle even without hours in the gym or highly restrictive diets. Join 1000+ students here.
2. Are you an entrepreneur who wants to get lean, boost energy, and get in your best shape? Apply for private one-on-one coaching here.
References
Chronic inflammation and disease
- Furman D et al. “Chronic inflammation in the etiology of disease across the life span.” Nature Medicine. 2019. (Links low‑grade chronic inflammation to cardiovascular disease, cancer, diabetes, depression, and frailty.)
- Franceschi C & Campisi J. “Chronic inflammation (inflammaging) and its potential contribution to age‑associated diseases.” Mechanisms of Ageing and Development. 2014. (Introduces “inflammaging” and connects chronic inflammation with multimorbidity and accelerated biological aging.)
- Guo J et al. “Aging and aging-related diseases: from molecular mechanisms to interventions.” Signal Transduction and Targeted Therapy. 2022. (Describes chronic inflammation as a key hallmark of aging and driver of organ decline.)
- “Chronic inflammation and the hallmarks of aging.” National Institutes of Health, 2023. (Reviews chronic inflammation as a central pathway linking aging to cardiovascular disease, dementia, diabetes, cancer, and frailty.)
Periodontal disease, bleeding gums, and systemic inflammation
- Machado V et al. “Serum C-Reactive Protein and Periodontitis: A Systematic Review and Meta-Analysis.” Frontiers in Immunology. 2021. (Periodontitis consistently associated with higher CRP/hs‑CRP; treatment reduces systemic inflammatory markers.)
- Lee JH et al. “Relationship between C-reactive protein level and periodontitis and systemic diseases.” Journal of Periodontology. 2024. (Links periodontal inflammation with elevated hs‑CRP and cardiometabolic comorbidities.)
- Hajishengallis G & Chavakis T. “Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities.” Nature Reviews Immunology. 2021. (Outlines how gum inflammation drives systemic low‑grade inflammation and chronic disease risk.)
Visceral fat, stubborn belly fat, and inflammation
- Kojta I et al. “Adipose tissue inflammation and metabolic dysfunction in obesity.” American Journal of Physiology – Cell Physiology. 2020. (Shows obese visceral fat secretes pro‑inflammatory cytokines and contributes to systemic low‑grade inflammation.)
- Chait A & den Hartigh LJ. “Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences.” Frontiers in Cardiovascular Medicine. 2020. (Explains how visceral fat is metabolically active, producing inflammatory mediators and driving cardiometabolic disease.)
- “Obese visceral fat tissue inflammation: from protective to detrimental?” 2022. (Narrative review on visceral adipose tissue inflammation and its systemic effects.)
Omega-3 fatty acids and inflammation
- Kavyani Z et al. “Efficacy of omega-3 fatty acids supplementation on inflammatory biomarkers: An umbrella meta-analysis.” International Immunopharmacology. 2022. (Omega‑3 supplementation reduces CRP and other inflammatory markers across multiple RCTs.)
- Calder PC. “Omega‑3 polyunsaturated fatty acids and inflammatory processes.” Nutrients. 2013. (EPA/DHA inhibit leukocyte chemotaxis, adhesion molecule expression, and production of TNF‑α, IL‑1β, IL‑6.)
- Lam M et al. “Omega 3 supplementation reduces C-reactive protein, prostaglandin E2 and the granulocyte/lymphocyte ratio in heavy smokers.” Frontiers in Nutrition. 2022. (Demonstrates omega‑3 lowering several inflammatory markers.)
- Fatima T et al. “Effectiveness of fish oil in controlling inflammation in adult patients undergoing hemodialysis.” SAGE Open Medicine. 2024. (Fish oil improves inflammatory profiles in a high‑risk population.)
Sleep, circadian alignment, and inflammation
- Irwin MR et al. “Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis.” Biological Psychiatry. 2016. (Short or fragmented sleep associates with higher CRP, IL‑6, TNF‑α.)
- Ballesio A et al. “Effects of Experimental Sleep Deprivation on Peripheral Inflammation: An Updated Meta-Analysis.” Journal of Sleep Research. 2025. (Acute sleep restriction increases inflammatory markers.)
- Ferrie JE et al. “The effect of sleep and its restriction on selected inflammatory parameters.” Scientific Reports. 2024. (Sleep restriction elevates hs‑CRP and other inflammatory markers.)
- “Immunological and inflammatory effects of infectious diseases in circadian rhythm disruption and future therapeutic directions.” 2023. (Reviews bidirectional links between circadian disruption and immune/inflammatory changes.)
Walking, low‑intensity movement, and post‑meal glucose
- Saint‑Maurice PF et al. “Association of Daily Step Count and Step Intensity With Mortality Among US Adults.” JAMA. 2020. (8,000+ steps/day linked to substantially lower all‑cause mortality vs 4,000; intensity less important than volume.)
- Bellini A et al. “The Effects of Postprandial Walking on the Glucose Response after Meals with Different Characteristics.” 2022. (30 minutes of brisk walking after meals improves postprandial glycemic response across meal types.)
- “Positive impact of a 10-min walk immediately after glucose intake on postprandial glucose levels.” Scientific Reports. 2025. (10‑minute walk immediately after glucose ingestion meaningfully blunts postprandial glucose vs sitting.)
Chronic stress, cortisol, and low‑grade inflammation
- Slavich GM. “Psychological stress and inflammation: A review of neuroimmune mechanisms and implications for health.” Annual Review of Clinical Psychology. 2016. (Details how chronic stress upregulates pro‑inflammatory signaling.)
- Miller GE et al. “A functional genomic perspective on human stress and disease.” Nature Reviews Immunology. 2007. (Chronic stress skews gene expression toward pro‑inflammatory profiles.)
- “Low-Grade Inflammation and Ambulatory Cortisol in Adolescents.” Psychosomatic Medicine. 2011. (Shows associations between chronic stress exposure, altered cortisol patterns, and low‑grade inflammation.)
Probiotics (including L. reuteri) and hs‑CRP
- Mazidi M et al. “Impact of Probiotic Administration on Serum C-Reactive Protein: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Nutrients. 2017. (Probiotics significantly reduce serum hs‑CRP overall.)
- “Lactobacillus reuteri V3401 reduces inflammatory biomarkers and improves metabolic syndrome components.” Nutrients. 2019. (L. reuteri strain in metabolic syndrome shows improvements in inflammatory/metabolic markers.)
- Söderberg Veibäck G et al. “A double-blind randomized placebo-controlled trial of Limosilactobacillus reuteri in patients with depression and low-grade inflammation.” 2025. (Explores L. reuteri’s anti‑inflammatory and mood effects in humans with hs‑CRP ≥1 mg/L.)
Vitamin D and inflammation
- Zhang Y et al. “Effects of vitamin D supplementation on inflammatory markers: a systematic review and meta-analysis.” Cytokine. 2018. (Vitamin D supplementation modestly reduces CRP and other inflammatory markers, especially in deficient individuals.)
- Calton EK et al. “Vitamin D status and inflammation: a systematic review of observational studies.” Current Pharmaceutical Design. 2015. (Low vitamin D status consistently associated with higher inflammatory markers.)
Magnesium and inflammation
- Simental‑Mendía LE et al. “Effect of magnesium supplementation on plasma C-reactive protein concentrations: A systematic review and meta-analysis of randomized controlled trials.” Current Pharmaceutical Design. 2017. (Magnesium supplementation reduces CRP in people with elevated baseline inflammation.)
- Asbaghi O et al. “Effect of Magnesium Supplementation on Inflammatory Parameters: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Nutrients. 2022. (Magnesium lowers CRP and other inflammatory markers in multiple RCTs.)
- “The effect of long-term magnesium intake on inflammatory markers in patients with metabolic syndrome: a systematic review and meta-analysis.” 2025. (Long‑term magnesium intake improves CRP, particularly over 12–16 weeks.)
Sauna / heat exposure, heat shock proteins, and inflammation
- Laukkanen T et al. “Association Between Sauna Bathing and Fatal Cardiovascular and All-Cause Mortality Events.” JAMA Internal Medicine. 2015. (Frequent sauna use associated with lower cardiovascular and all‑cause mortality; mechanisms include blood pressure and inflammation changes.)
- Singh IS & Hasday JD. “Fever, hyperthermia and the heat shock response.” International Journal of Hyperthermia. 2013. (Explains how heat stress induces heat shock proteins that modulate inflammatory pathways.)
- “The Hidden Power of Heat Shock Proteins.” (Educational overview on sauna‑induced HSPs, autophagy, and reduced oxidative stress/inflammatory damage.)
Cold exposure and inflammatory markers
- Bleakley CM & Davison GW. “What is the biochemical and physiological rationale for using cold-water immersion in sports recovery? A systematic review.” British Journal of Sports Medicine. 2010. (Cold water immersion reduces some inflammatory mediators and DOMS in athletes.)
- Poppendieck W et al. “Cooling and performance recovery of trained athletes: a meta-analytical review.” BMJ Open Sport & Exercise Medicine. 2013. (Cold exposure can attenuate markers of muscle damage and inflammation post‑exercise.)
- “Ice Baths for Chronic Inflammation: Evidence-Based Approach.” 2025. (Summarizes human and animal data showing cold exposure can reduce pro‑inflammatory cytokines such as IL‑6 and TNF‑α.)
Nasal vs mouth breathing, sleep, and inflammation
- Guglielmi O et al. “Obstructive sleep apnea, cardiovascular disease, and inflammation.” European Journal of Internal Medicine. 2010. (Sleep‑disordered breathing linked with systemic inflammation and elevated CRP, IL‑6.)
- Malhotra A & Owens RL. “What is central sleep apnea?” Respiratory Care. 2010. (Discusses how airway collapse and mouth breathing relate to disrupted sleep and cardiometabolic stress.)
- “How mouth and nasal breathing affect snoring and sleep apnea.” SleepHealthy PA. 2025. (Clinical explanation of nasal breathing improving airway stability, oxygenation, and sleep quality vs mouth breathing.)
Alcohol, gut permeability, and inflammation
- Bishehsari F et al. “Alcohol and Gut-Derived Inflammation.” Alcohol Research: Current Reviews. 2017. (Alcohol increases intestinal permeability, endotoxemia, and systemic inflammation.)
- Kirpich IA & McClain CJ. “Probiotic therapy in alcoholic liver disease.” Journal of Gastroenterology and Hepatology. 2012. (Details alcohol‑induced gut barrier dysfunction and inflammatory responses.)
- Varela‑Rey M et al. “Pathogenesis of alcoholic liver disease: an overview.” World Journal of Gastroenterology. 2013. (Even moderate drinking can increase gut permeability and inflammatory signaling.)
hs-CRP risk thresholds
- Pearson TA et al. “Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice.” Circulation. 2003. (CDC/AHA joint guidelines: <1.0 mg/L low risk; 1.0–3.0 average; >3.0 high.)
- Centers for Disease Control and Prevention / American Heart Association. “Use of high sensitivity C‑reactive protein in assessing cardiovascular disease risk.” (Consensus statement using tertile cut‑offs: <1.0, 1.0–3.0, >3.0 mg/L.)
Disclaimer: This email is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease, and those seeking personal medical advice should consult with a licensed physician.